Case
36 Diagnosis and discussion |
Versión
en Español |
|||
Go back to clinical information and images
Diagnosis: Antibody mediated rejection (AMR) (suspicious for or presumptive)
The central diagnostic criteria today of antibody-mediated rejection (AMR) - or humoral rejection - are the demonstration of C4d in peritubular capillaries and inflammation and/or tissue injury (Terasaki P, Mizutani K. Clin J Am Soc Nephrol. 2006;1(3):400-3. [PubMed link] [Free full text]). Even so, according to Bannf's consensus classification of renal allograft rejection (2007), diagnosis requires "documentation of circulating antidonor antibodies"; cases that meet only two of the three criteria are considered "suspicious for".
The three criteria are: morphologic evidence (acute tubular injury, neutrophils and/or mononuclear cells in peritubular capilaries and/or glomeruli and/or capillary thrombosis, fibrinoid necrosis/intramural or transmural inflammation in arteries), immunopathologic evidence (C4d or immunoglobulins deposition in peritubular capilaries), and serologic evidence (anti-donor antibodies).
Three forms of antibody-mediated graft injury have been defined: Hyperacute rejection, acute humoral rejection, and chronic humoral rejection. A fourth "form of rejection" has been proposed for Robert B. Colvin: "accomodation" (i.e. normal graft function with normal or almost normal renal histology, and C4d deposition in peritubular capillaries).
Patients with acute AMR present with an acute loss of graft function that often arises in the first few weeks after transplantation and cannot be distinguished from cell-mediated rejection on clinical grounds. AMR can also develop years after transplantation, often triggered by a decrease in immunosuppression (iatrogenic, noncompliance, or malabsorption). Presensitization is the major risk factor, but most of the patients with AMR had a negative cross-match. AMR has occurred with all immunosuppression regimens, even profoundly depleting therapy (Colvin RB. J Am Soc Nephrol. 2007;18(4):1046-56. [PubMed link] [Free full text]).
Renal biopsies may show acute cellular rejection, acute tubular injury, or thrombotic microangiopathy
In the present case, vascular involvement is also evidenced by parenchymal hemorrhagic necrosis (see below the Figure 11). With methenamine silver staining glomerular and arteriolar microthrombi are better evidenced (Figure 12, below).
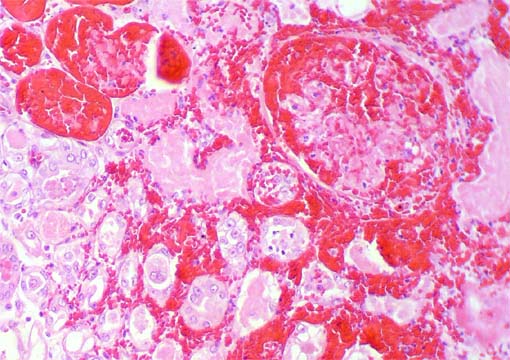
Figure 11. H&E, X200.
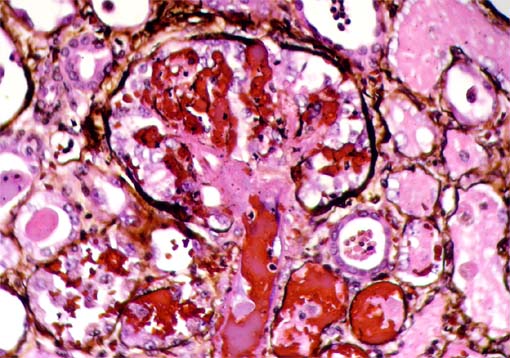
Figure 12. Methenamine-silver stain, X400.
See the chapter Transplantation Pathology of our Tutorial (at present there is only a Spanish version).
Go back to clinical information and images
Bibliography
-
Yang YW, Lin WC, Wu MS, Lee PH, Tsai MK. Early diagnosis and successful treatment of acute antibody-mediated rejection of a renal transplant. Exp Clin Transplant. 2008;6(3):211-4. [PubMed link] [Free full text]
- Solez K, Colvin RB, Racusen LC, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant. 2008;8(4):753-60. [PubMed link]
-
Colvin RB. Antibody-mediated renal allograft rejection: diagnosis and pathogenesis. J Am Soc Nephrol. 2007;18(4):1046-56. [PubMed link] [Free full text]
-
Banasik M, Boratynska M, Nowakowska B, Halon A, Koscielska-Kasprzak K, Drulis-Fajdasz D, Patrzalek D, Weyde W, Klinger M. C4D deposition and positive posttransplant crossmatch are not necessarily markers of antibody-mediated rejection in renal allograft recipients. Transplant Proc. 2007;39(9):2718-20. [PubMed link]
- Akalin E, Watschinger B. Antibody-mediated rejection. Semin Nephrol. 2007;27(4):393-407. [PubMed link]
-
Racusen LC, Haas M. Antibody-mediated rejection in renal allografts: lessons from pathology. Clin J Am Soc Nephrol. 2006;1(3):415-20. [PubMed link] [Free full text]
-
Terasaki P, Mizutani K. Antibody mediated rejection: update 2006. Clin J Am Soc Nephrol. 2006;1(3):400-3. [PubMed link] [Free full text]